

A “tongue-tie,” otherwise known as ankyloglossia, is an excessive soft-tissue adhesion on the underside of the tongue, which may result in restriction of tongue movement or position depending on severity. Ankyloglossia is not well understood by many in the medical and dental community, however, our doctors recognize the problems this tethering of the tongue can cause and we are here to help.
Our doctors recognize the problems this tethering of the tongue can cause and we are here to help.

Our doctors recognize the potential for this small tethering of the tongue to cause or contribute to a worsening of many conditions including mouth breathing, reoccurring ear/throat infections and need for ear tubes, jaw growth and development, snoring, sleep apnea and anxiety, to name a few.
There are two types of tongue-ties, anterior and posterior. A Google image search will show hundreds of examples of tongue-ties. What you see in these images are anterior tongue-ties. A posterior tongue-tie is more difficult to appreciate visually, as it is deeper within the soft tissue of the tongue. Both anterior and posterior tongue-ties can contribute to airway dysfunction.
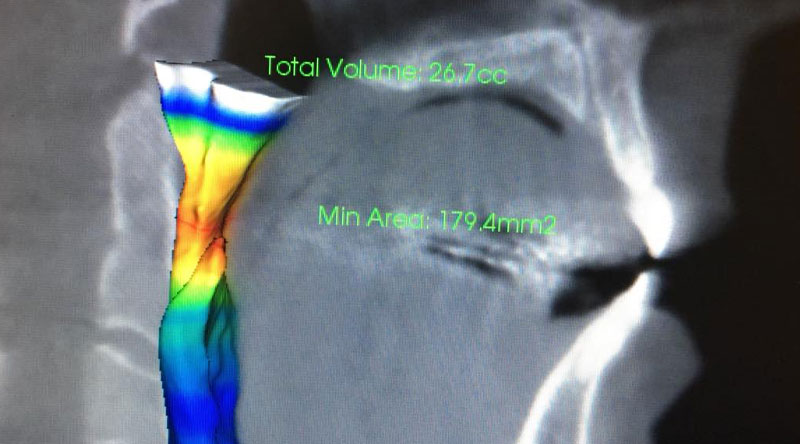
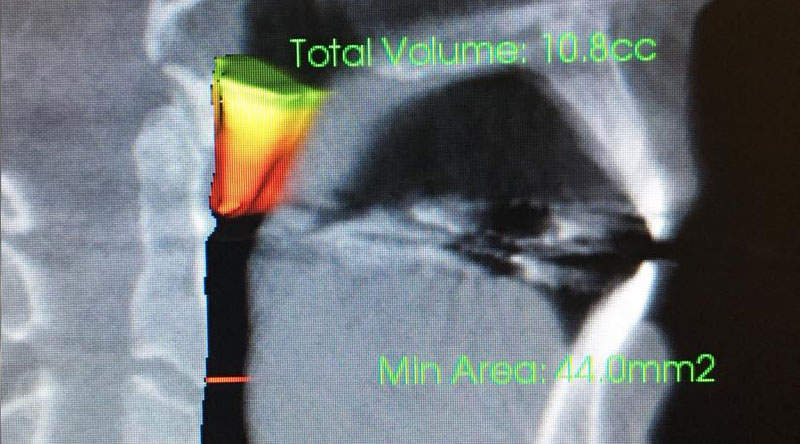
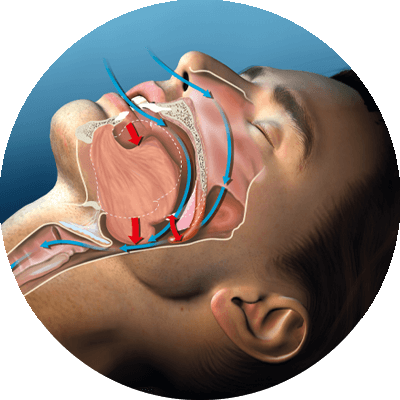
Our airway is a soft-sided tube that runs from our nose down to our lungs which allows us to bring oxygen to our body’s cells. It is important to understand that the mouth is not part of our airway. The flow through our airway changes based on the internal volume. When it comes to the airway, slight changes in volume can have a dramatic impact on the flow of air. There are multiple points where you can end up with a kink, and in many cases these kinks lead to changes in the restorative quality of our sleep. A tongue-tie is just one, albeit quite common, of these points.
When a tongue-tie creates an airway disturbance, our brains initially compensate by altering our sleep cycle to avoid the more relaxed portions of it. Over time, our brains become conditioned to the inadequate airflow, and eventually, our brains allow periods of apnea (a lack of breathing). This is the terminal stage of sleep-disordered breathing — obstructive sleep apnea — which can lead to death if left untreated.
Another common result from a low tongue position is mouth breathing. The nasal cavity filters particulate matter, including bacteria and viruses, out of the air we breathe. While filtering, we secrete a powerful substance called nitric oxide to kill these bacteria/viruses and further protect our bodies from foreign invaders.
The large surface area inside our nasal cavity also moistens the air we breathe. A moistened airway is a healthy airway. When we breathe through our mouths, we lose these protections. Bacteria and viruses bypass the death trap of our nasal cavity and gain easy access into our bodies through this damaged lining, which leads to frequent upper respiratory infections. The tonsils enlarge in the process of eliminating the extra load of bacteria and viruses that they aren’t being eliminated in the nose.
In addition to frequent upper respiratory infections, those with tongue-ties are at an elevated risk for middle ear infections. The middle ear connects to the throat via the eustachian tube. The eustachian tubes may not function properly when swallowing is altered by a tongue-tie, or the tonsils are enlarged from mouth breathing.
Tongue-ties can have significant effects on the growth and development of the jaws. The lips and cheeks create an elastic force pulling back against the outward and forward growth of the jaws. When the tongue is not in the palate to provide the counterbalance to this force, jaw growth is unable to progress normally. The lack of outward growth results in a narrow nasal airway.
Corrective action for a tongue-tie consists of two necessary components — lingual frenectomy (surgical release) and oral myofunctional therapy (like physical therapy for your tongue).
Oral myofunctional therapy (OMT) begins before surgery and involves a series of progressing exercises to strengthen the tongue and prepare for its release. OMT is individualized to the patient, so the duration and exercises will vary from patient to patient. Once adequately prepared, your therapist will release you or your child to proceed with the lingual frenectomy.
A lingual frenectomy is typically done under local anesthesia for adults, though intravenous sedation is available as needed for patient comfort. In children, the procedure is typically performed under sedation to eliminate tongue movement.

There are generally two situations where medical insurers will provide coverage for a lingual frenectomy, an infant having difficulty breastfeeding with a letter of necessity from a lactation consultant, or an older child with a letter of necessity from a speech pathologist.
I understand the information disclosed in this form may be subject to re-disclosure and may no longer be protected by HIPAA privacy regulations and the HITECH Act.
